 A study published in Annals of Internal Medicine has found that men with a stressful job are twice as likely to have a stroke than are men with less demanding jobs. Interestingly, there was no correlation between job stress and incidence of stroke among women.
A study published in Annals of Internal Medicine has found that men with a stressful job are twice as likely to have a stroke than are men with less demanding jobs. Interestingly, there was no correlation between job stress and incidence of stroke among women.
A stroke occurs when the blood supply to the brain is cut off, for example when a clot blocks one of the blood vessels supplying the brain. Stroke can cause permanent neurological damage and even death, and has been linked to stress for quite some time.
Tsutsumi et al. interviewed 3,190 Japanese men and 3,363 Japanese women from a variety of job backgrounds, including managers, professionals, technicians, clerks, salespeople, farmers, craftsmen and labourers. The level of occupational stress experienced by these workers was evaluated and participants were placed into four stress categories: high strain (high job demand + low job control); active job (high job demand + high job control); low strain (low job demand + high job control); and passive job (low job demand + low job control).
Over the next 11 years, 91 men and 56 women experienced a stroke. Men under high job strain – i.e. those with lots of demands on their shoulders and with little control of their workload – were twice as likely to experience a stroke than were men under low strain. In women, however, the incidence of stroke was the similar among those with a stressful job and those under less strain.
Among men, the association between job stress and stroke lessened somewhat when other risk factors for stroke, such as obesity and high blood pressure, were taken into account, suggesting that pre-existing chronic diseases and an unhealthy lifestyle up the chance of stroke in stressed out employees.
The authors of the study suggest that that the difference between the sexes could be because women approach stressful jobs differently to men or because more women than men work part-time.
————————————————————————————————-
Akizumi Tsutsumi, Kazunori Kayaba, Kazuomi Kario, and Shizukiyo Ishikawa (2009) Prospective Study on Occupational Stress and Risk of Stroke Arch Intern Med 169 (1): 56-61

 A study of nearly 1,400 adult and pediatric cancer patients
A study of nearly 1,400 adult and pediatric cancer patients 
 Mobile phones are possibly one of the most ubiquitous pieces of technology in the 21st century. In 2003 the
Mobile phones are possibly one of the most ubiquitous pieces of technology in the 21st century. In 2003 the 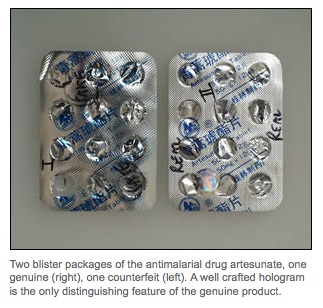 An orchestrated raid in ten countries has led to
An orchestrated raid in ten countries has led to  A
A  One in four 4-5 year old children and one in three 10-11 year olds in England are obese or overweight, according to
One in four 4-5 year old children and one in three 10-11 year olds in England are obese or overweight, according to  Every year the
Every year the  In the recent US election, several pieces of legislation that aimed to limit reproductive rights were voted down. Colorado said no to the
In the recent US election, several pieces of legislation that aimed to limit reproductive rights were voted down. Colorado said no to the 